Fact Sheet
Prevention of late-onset sepsis including the use of an exclusive human milk diet technical bulletin
Technical Bulletin
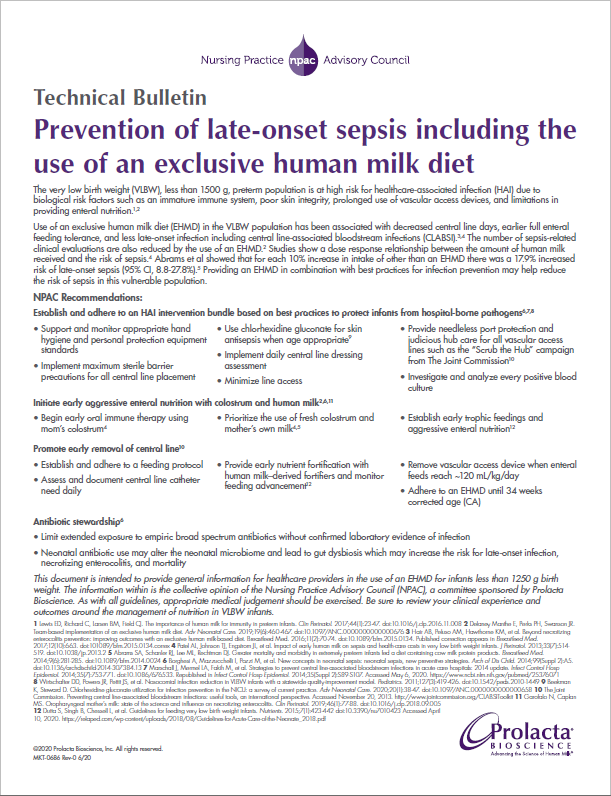
Prevention of late-onset sepsis including the use of an exclusive human milk diet
The very low birth weight (VLBW), less than 1500 g, preterm population is at high risk for healthcare-associated infection (HAI) due to biological risk factors such as an immature immune system, poor skin integrity, prolonged use of vascular access devices, and limitations in providing enteral nutrition.1,2
Use of an exclusive human milk diet (EHMD) in the VLBW population has been associated with decreased central line days, earlier full enteral feeding tolerance, and less late-onset infection including central line-associated bloodstream infections (CLABSI). 3,4 The number of sepsis-related clinical evaluations are also reduced by the use of an EHMD.2 Studies show a dose response relationship between the amount of human milk received and the risk of sepsis.4 Abrams et al showed that for each 10% increase in intake of other than an EHMD there was a 17.9% increased risk of late-onset sepsis (95% CI, 8.8-27.8%).5 Providing an EHMD in combination with best practices for infection prevention may help reduce the risk of sepsis in this vulnerable population.
NPAC Recommendations:
Establish and adhere to an HAI intervention bundle based on best practices to protect infants from hospital-borne pathogens6,7,8
- Support and monitor appropriate hand hygiene and personal protection equipment standards
- Implement maximum sterile barrier precautions for all central line placement
- Use chlorhexidine gluconate for skin antisepsis when age appropriate9
- Implement daily central line dressing assessment
- Minimize line access
- Provide needleless port protection and judicious hub care for all vascular access lines such as the “Scrub the Hub” campaign from The Joint Commission10
- Investigate and analyze every positive blood culture
Initiate early aggressive enteral nutrition with colostrum and human milk2,6,11
- Begin early oral immune therapy using mom’s colostrum4
- Prioritize the use of fresh colostrum and mother’s own milk4,5
- Establish early trophic feedings and aggressive enteral nutrition12
Promote early removal of central line10
- Establish and adhere to a feeding protocol
- Assess and document central line catheter need daily
- Provide early nutrient fortification with human milk–derived fortifiers and monitor feeding advancement12
- Remove vascular access device when enteral feeds reach ~120 mL/kg/day
- Adhere to an EHMD until 34 weeks corrected age (CA)
Antibiotic stewardship6
- Limit extended exposure to empiric broad spectrum antibiotics without confirmed laboratory evidence of infection
- Neonatal antibiotic use may alter the neonatal microbiome and lead to gut dysbiosis which may increase the risk for late-onset infection, necrotizing enterocolitis, and mortality
This document is intended to provide general information for healthcare providers in the use of an EHMD for infants less than 1250 g birth weight. The information within is the collective opinion of the Nursing Practice Advisory Council (NPAC), a committee sponsored by Prolacta Bioscience. As with all guidelines, appropriate medical judgement should be exercised. Be sure to review your clinical experience and outcomes around the management of nutrition in VLBW infants.
1 Lewis ED, Richard C, Larsen BM, Field CJ. The importance of human milk for immunity in preterm infants. Clin Perinatol. 2017;44(1):23-47. doi:10.1016/j.clp.2016.11.008
2 Delaney Manthe E, Perks PH, Swanson JR. Team-based implementation of an exclusive human milk diet. Adv Neonatal Care. 2019;19(6):460-467. doi:10.1097/ANC.0000000000000676
3 Hair AB, Peluso AM, Hawthorne KM, et al. Beyond necrotizing enterocolitis prevention: improving outcomes with an exclusive human milk-based diet. Breastfeed Med. 2016;11(2):70-74. doi:10.1089/bfm.2015.0134. Published correction appears in Breastfeed Med. 2017;12(10):663. doi:101089/bfm.2015.0134.correx
4 Patel AL, Johnson TJ, Engstrom JL, et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol. 2013;33(7):514- 519. doi:10.1038/jp.2013.2
5 Abrams SA, Schanler RJ, Lee ML, Rechtman DJ. Greater mortality and morbidity in extremely preterm infants fed a diet containing cow milk protein products. Breastfeed Med. 2014;9(6):281-285. doi:10.1089/bfm.2014.0024
6 Borghesi A, Mazzucchelli I, Pozzi M, et al. New concepts in neonatal sepsis: neonatal sepsis, new preventive strategies. Arch of Dis Child. 2014;99(Suppl 2):A5. doi:10.1136/archdischild-2014-307384.13
7 Marschall J, Mermel LA, Fakih M, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(7):753-771. doi:10.1086/676533. Republished in Infect Control Hosp Epidemiol. 2014;35(Suppl 2):S89-S107. Accessed May 6, 2020. https://www.ncbi.nlm.nih.gov/pubmed/25376071
8 Wirtschafter DD, Powers JR, Pettit JS, et al. Nosocomial infection reduction in VLBW infants with a statewide quality-improvement model. Pediatrics. 2011;127(3):419-426. doi:10.1542/peds.2010-1449
9 Beekman K, Steward D. Chlorhexidine gluconate utilization for infection prevention in the NICU: a survey of current practice. Adv Neonatal Care. 2020;20(1):38-47. doi:10.1097/ANC.0000000000000658
10 The Joint Commission. Preventing central line-associated bloodstream infections: useful tools, an international perspective. Accessed November 20, 2013. http://www.jointcommission.org/CLABSIToolkit
11 Garofalo N, Caplan MS. Oropharyngeal mother’s milk: state of the science and influence on necrotizing enterocolitis. Clin Perinatol. 2019;46(1):77-88. doi:10.1016/j.clp.2018.09.005
12 Dutta S, Singh B, Chessell L, et al. Guidelines for feeding very low birth weight infants. Nutrients. 2015;7(1):423-442 doi:10.3390/nu7010423 Accessed April 10, 2020. https://relaped.com/wpcontent/uploads/2018/08/Guidelines-for-Acute-Care-of-the-Neonate_2018.pdf
